How to Clean Medical Claims?
It’s no news that medical billing company are rejecting far more claims than they were a year or two ago. To avoid long delays or nonpayment, practices must devote more time and effort to proper filings. An industry expert discusses why things have changed and offers actionable advice you can apply right now to lessen or even eliminate denials.
Claims Denials Problems:
It’s enormous. Each denial will set you back around $15. However, every time a claim is denied, your chances of collecting full reimbursement are diminished. Managing second and third resubmissions is substantially more complex than collecting original submissions. To make matters worse, a patient’s cost-share is typically not invoiced until insurance kicks in. The longer the time between care and billing, the less likely the patient will pay.
What’s going on with patient copays and deductibles?
In 2022, this will be another area of significant change. Many services, like Covid-19 therapy, are no longer fully covered by most Medical Billing companies. Patients are facing substantially larger bills than in the past. Patients are notoriously difficult payers, so this is poor news for physicians. The landscape is changing so quickly that billers frequently have no idea how much a deductible or copay will be at the start of patient interaction. We’ll have to wait till the medical billing insurance company responds. As a result, we are at a disadvantage. It’s tough to estimate or collect the patient’s portion early on in the procedure when it’s the most efficient.
How Can Medical Billing Company and Practices Prevent from Denials?
The entire game has shifted. Before now, timely submissions were the key to timely and complete payments. The focus is now on accuracy. Because claims must be flawless, submitters face a significant challenge. The bar has been set extremely high. The adage holds when it comes to claims processing. Because people are being phased out of the insurance sector, any minor inaccuracy on the submitter is likely to be spotted by super-efficient computer auditing functions.
A biller’s task is to clean up any ‘trash’ or errors. Automation at the provider’s end improves accuracy as well. Business intelligence is significantly more manageable with a sophisticated billing system with integrated reporting. Then pay close attention to all of the system’s alarms. I’ve observed far too many people ignore alerts, oblivious that the “annoying” flashing light may be preventing them from submitting errors.
How Can Medical Billing Company Know That Patient Pay their Share?
They can keep patients satisfied. According to one survey, pleased customers pay their bills 74% of the time and return for future service 95% of the time. On the other hand, dissatisfied patients only pay 33% of the time, and just 58 percent say they would return. According to 45 percent of those polled, the worst portion of the patient trip was post-visit services (billing, insurance, follow-up, etc).
Suggestions Improving Patient Engagement:
Whether internal or outsourced, practices must embrace their billing personnel. Many internal back-office departments are consigned to a basement or a windowless structure area. Too many outsourced billing organizations are regarded as outsiders, even though the revenue they generate sustains the entire operation. If everyone in the office feels like they’re part of the same team, they’ll collaborate to improve the patient experience. Front-office administrators, for example, are less likely to make mistakes when collecting registration and eligibility information if they are familiar with billing concerns. Patients are happy when there are fewer billing errors, and they are more inclined to pay their fair share.
Patient satisfaction should be a source of accountability for the employee, and it’s even better if it can be included in their annual review. While it’s true that most billing departments are chronically understaffed, I believe that practice owners will see a direct link between adding a Patient Financial Experience role and revenue cycle improvements, which will more than justify the staffing investment.
What else can practices do to guarantee that their statements are more accurate?
While the claim is still in their possession, practitioners must strive for 100 percent accuracy. This is the area in which you have the most power. They can make the most of their systems’ features, such as a claims scrubber. Patients can provide their insurance and demographic information through the patient portal, which is available in many EHRs today. They can also keep an ear to the ground and spot trends. Every rejection or denial should be investigated and reported to the practice’s Denial Prevention Director. Each rejection or denial should be detailed in a weekly denial report, including the volume, cash value, and message connected with each rejection or refusal.
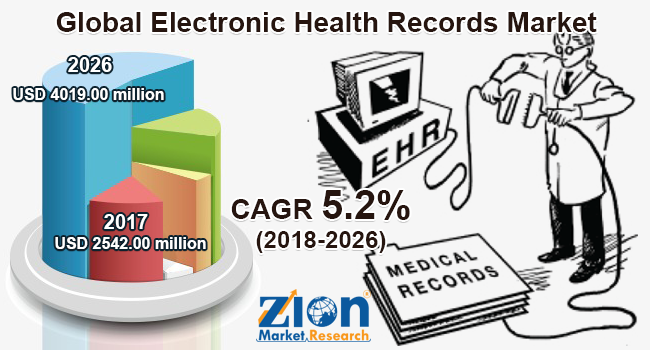
Bellmedex is a Best Medical Billing Company based in the United States that provides skilled practice management, electronic health records, and top medical billing services for faster claims processing and higher reimbursements. You can keep track of and manage your practice on the move with BellMedex comprehensive spectrum of services and sophisticated EHR. Our dependable services optimize operations and provide efficient practice management by automating workflows and claims processes.
Detailed reports allow you to spot patterns with specific insurers, alerting you to potential software flaws. About half of denials are caused by practice errors that can be corrected, and insurance policies cause the other half. If you feel an insurer denies claims unreasonably, contact the payer or file a complaint with your state’s insurance commissioner.